When an Earache Is More Than Just a Nuisance
Ear infections are often thought of as a childhood issue—but they can strike adults too, and when they do, the consequences can be far more serious than a few days of discomfort. What begins as a mild ache or muffled hearing can sometimes lead to long-term consequences—including permanent hearing loss.
For many adults, it’s easy to dismiss an ear infection as “no big deal,” especially if you’ve had one before. But repeated infections, improper treatment, or underlying conditions can all turn a temporary problem into a lasting impairment.
So, can ear infections in adults lead to permanent hearing loss? The answer is yes—but it’s not inevitable. With timely care and a better understanding of the risks, many complications can be prevented.
In this article, we’ll explore the types of adult ear infections, how they affect your hearing, the conditions that raise your risk of permanent damage, and what to do if you notice hearing changes after an infection. Whether you’re dealing with an ear problem now or looking to prevent future issues, this guide will help you protect your hearing—before it’s too late.
Understanding Adult Ear Infections
While ear infections are more common in children, they can—and do—occur in adults. And when they strike, they often come with stronger symptoms and a higher risk of complications due to delayed treatment or underlying health issues.
Types of Ear Infections in Adults
There are several types of ear infections that can affect adults, each with different causes and consequences:
Otitis Media (Middle Ear Infection):
Often caused by bacteria or viruses, this type leads to inflammation behind the eardrum. It may cause fluid buildup, pressure, and temporary hearing loss. Chronic or repeated infections can damage structures in the middle ear.Otitis Externa (Outer Ear Infection or “Swimmer’s Ear”):
Usually caused by bacteria or fungi entering the ear canal, often after water exposure. While it rarely affects hearing permanently, severe or untreated cases can damage the ear canal and eardrum.Inner Ear Infections (Labyrinthitis or Vestibular Neuritis):
These are less common but more serious, as they can affect balance and cause sudden sensorineural hearing loss. Often viral in origin, they require immediate medical attention.Chronic Suppurative Otitis Media (CSOM):
A persistent middle ear infection with ongoing discharge, typically from a perforated eardrum. This can lead to permanent hearing loss and other complications if left untreated.
Symptoms and Causes to Watch For
Common signs of an ear infection in adults include:
Ear pain or fullness
Drainage from the ear
Muffled or reduced hearing
Dizziness or loss of balance
Fever and general malaise
Infections may stem from:
Upper respiratory illnesses
Allergies or sinus infections
Water trapped in the ear
Poor ear hygiene or aggressive cleaning
Understanding what kind of infection you have—and what caused it—can help you and your healthcare provider choose the right treatment and avoid long-term consequences.
How Ear Infections Affect Hearing
When it comes to hearing, even a minor infection can cause noticeable changes in how sound is perceived. While many ear infections result in temporary hearing loss, repeated or improperly treated cases can lead to long-term or permanent damage—especially if the inner or middle ear is involved.
Temporary vs Permanent Hearing Loss
Most ear infections cause temporary hearing loss due to:
Fluid buildup behind the eardrum (in otitis media)
Swelling of the ear canal (in otitis externa)
Pressure or blockage that prevents sound from traveling normally
Once the infection resolves and inflammation subsides, hearing usually returns to normal. However, certain conditions can tip the balance toward permanence.
The Role of Inflammation and Fluid Buildup
Inflammation is a double-edged sword—it helps fight infection, but it can also:
Thicken middle ear tissues
Cause scarring or stiffening of the eardrum
Lead to fluid accumulation that doesn’t drain properly
Promote bone erosion in long-term infections (as seen in CSOM)
These structural changes can reduce the conductive ability of the middle ear, making it harder for sound to reach the inner ear clearly—even after the infection clears.
In more severe cases, bacteria or viruses can spread into the cochlea or auditory nerve, damaging delicate sensory cells and causing sensorineural hearing loss, which is often permanent and irreversible.
The next section will explore when and how temporary hearing loss becomes permanent, and what signs indicate the need for urgent medical evaluation.
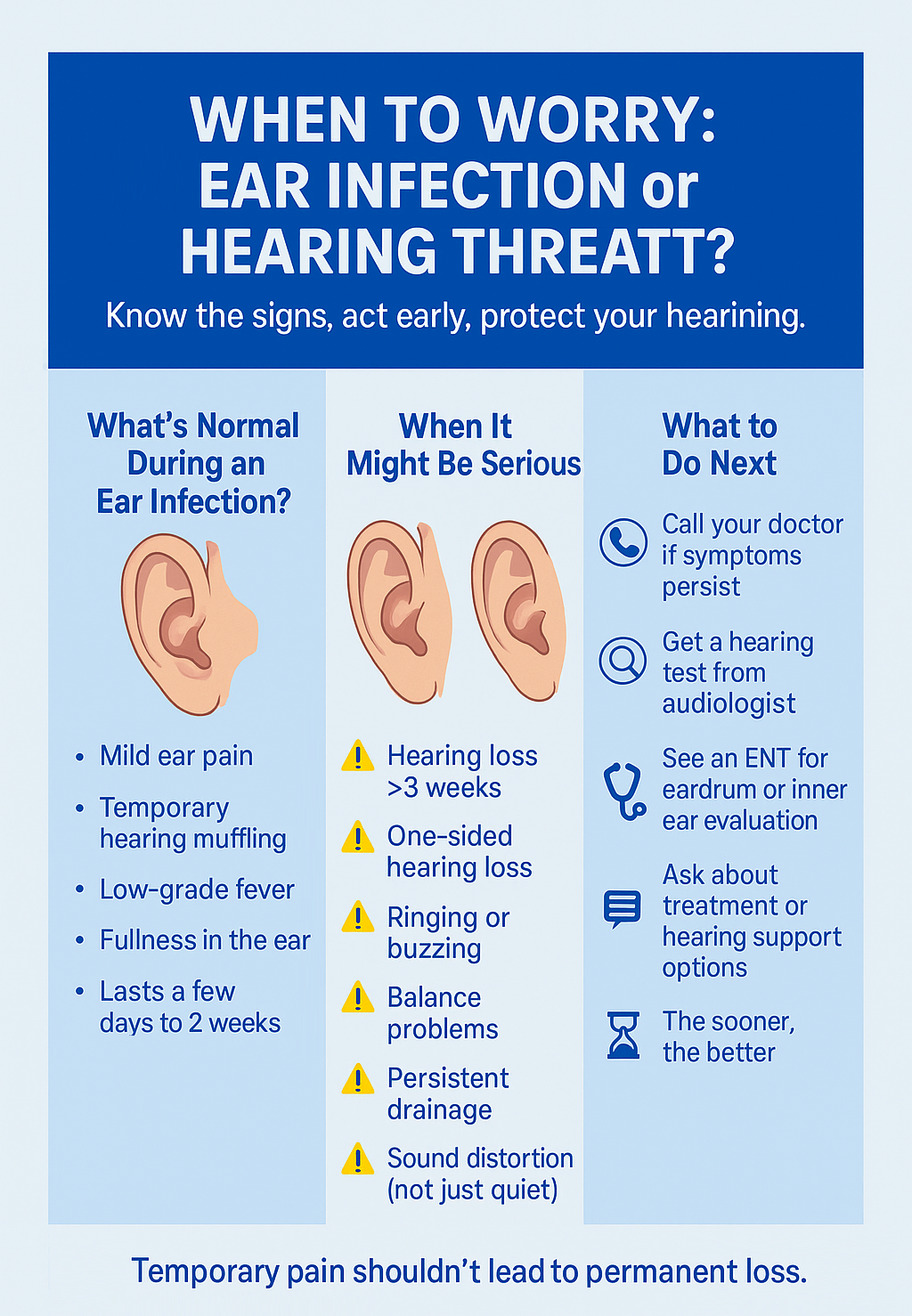
When Does Hearing Loss Become Permanent?
While most ear infections clear up without lasting damage, certain cases can result in irreversible hearing loss—especially when infections are chronic, severe, or improperly treated. Understanding the risk factors can help you take action before temporary symptoms become permanent.
Risk Factors for Long-Term Damage
The risk of permanent hearing loss increases if:
The infection spreads to the inner ear, damaging sensory hair cells
The eardrum ruptures or is perforated multiple times
There is recurrent or chronic otitis media that leads to scarring or ossicle damage
Hearing loss lasts more than 3–4 weeks after the infection clears
The infection is associated with cholesteatoma, an abnormal skin growth that erodes ear structures
There is an underlying health condition (e.g., diabetes, autoimmune disorders, immune suppression)
Repeated middle ear infections can also cause ossicular chain disruption, where the tiny bones in the ear become misaligned or eroded—leading to conductive hearing loss that may require surgical correction.
Chronic Infections, Ruptured Eardrums, and More
A single eardrum rupture often heals on its own. But repeated ruptures or one that doesn’t heal properly can lead to:
Ongoing drainage
Tinnitus (ringing in the ears)
Hearing distortion or permanent reduction
If you experience persistent hearing loss, especially after symptoms of an ear infection subside, this may indicate sensorineural damage—often caused by inner ear infection, inflammation, or delayed treatment.
Warning signs that hearing loss may be permanent include:
Loss in one ear only (asymmetrical hearing)
No improvement weeks after infection resolves
Sudden hearing drop accompanied by dizziness or ringing
Speech and sounds feel distorted, not just quiet
These symptoms require prompt evaluation by an audiologist or ENT specialist.
In the next section, we’ll explore how to treat infections effectively and prevent long-term damage through care and prevention.
Treatment Options and Prevention Tips
The good news is that most ear infections—when caught early—can be treated effectively, greatly reducing the risk of long-term hearing loss. Whether you’re managing symptoms now or want to avoid future infections, the right combination of medical care and prevention is key.
Medical Interventions and Home Care
Treatment depends on the type and severity of the infection, but common approaches include:
Antibiotics (oral or ear drops): Used for bacterial infections, especially when symptoms are moderate to severe or don’t improve within a few days.
Steroid ear drops: Often used for outer ear infections to reduce inflammation and itching.
Pain relievers: Over-the-counter medications like ibuprofen or acetaminophen help relieve pain and reduce fever.
Ear wicking or suction: For outer ear infections with significant drainage or blockage.
Tympanostomy (ear tubes): In chronic or recurrent middle ear infections, tubes may be surgically inserted to help drain fluid and equalize pressure.
Surgical repair: In rare cases of persistent eardrum perforation or ossicle damage, procedures like tympanoplasty or ossiculoplasty may be needed.
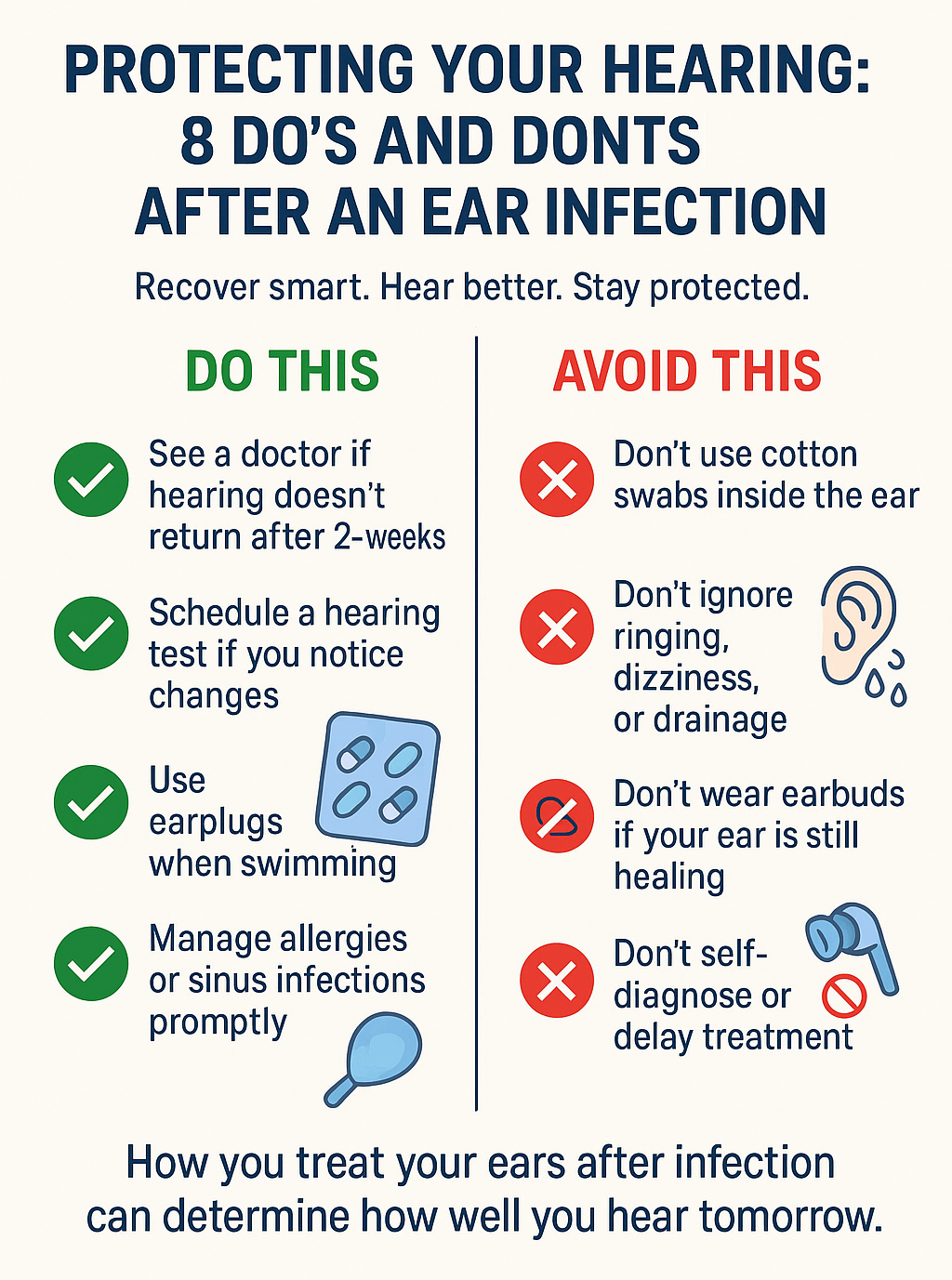
Never insert cotton swabs or foreign objects into your ears, especially during or after an infection, as this can worsen the problem or delay healing.
How to Avoid Complications and Protect Your Hearing
Prevention plays a powerful role in protecting long-term hearing. Here’s how to reduce your risk of adult ear infections and related damage:
Treat colds, sinus infections, and allergies promptly to reduce fluid buildup in the ears
Avoid smoking and secondhand smoke, which increase infection risk
Dry your ears thoroughly after swimming or showering
Use earplugs when swimming, especially in lakes or public pools
Manage chronic health conditions that affect immune response
Keep up with hearing checks if you’ve had repeated infections or hearing issues
Avoid using headphones or earbuds during an active infection, which can trap moisture and bacteria
Being proactive about ear health now can save your hearing later.
Next up, we’ll explore what to do if you notice hearing loss after an ear infection, including the next steps for testing and treatment.
What to Do If You Notice Hearing Loss After an Infection
Noticing muffled hearing, ringing in your ears, or difficulty following conversations after an ear infection? Don’t wait it out—early evaluation and treatment are your best chances of recovery or preservation.
When to Seek Help
While some hearing loss during an ear infection is normal, it should resolve within a few days to a couple of weeks. You should contact a healthcare provider if:
Your hearing doesn’t return after 2–3 weeks
You notice one-sided hearing loss
Sounds seem distorted or unclear, not just quieter
There’s ringing, buzzing, or a feeling of fullness in the ear
You experience dizziness or balance issues
There’s persistent drainage from the ear, even without pain
These could indicate inner ear involvement, nerve damage, or structural problems that require specialist care.
Hearing Tests, ENT Referrals, and Recovery Options
If symptoms persist, your doctor may refer you to:
An audiologist for a comprehensive hearing test (audiogram)
An ENT (ear, nose, and throat specialist) to examine your eardrum, check for structural damage, or assess for chronic infection
Depending on the cause and severity, treatment options may include:
Medication (for residual infection or inflammation)
Hearing aids or assistive listening devices (for permanent damage)
Surgery to repair perforated eardrums or damaged ossicles
Vestibular therapy (if balance is affected)
The earlier you get checked, the more options you’ll have for both treatment and hearing preservation.
Remember: untreated hearing loss can impact mental health, social connection, cognitive function, and quality of life. Don’t assume it’s “just part of getting older”—get it checked and addressed.
Conclusion: Take Ear Health Seriously – Because Hearing Loss Isn’t Always Temporary
Ear infections in adults are often brushed off as minor or temporary, but the truth is that they can lead to lasting damage—including permanent hearing loss. What starts as discomfort or muffled sound can escalate into long-term consequences if left untreated or repeated over time.
The key is awareness. By understanding the risks, symptoms, and warning signs, you’re already ahead of the curve. Early treatment, proper care, and preventive habits can protect your hearing for the long haul—and if something doesn’t feel right, don’t wait to get it checked out.
Your ears are not just for hearing—they’re for connection, safety, communication, and quality of life. Treat them with care, and they’ll serve you well for decades to come.
Frequently Asked Questions
Can one ear infection cause permanent hearing loss?
Yes, in rare cases. A severe or improperly treated infection can lead to complications such as eardrum rupture, chronic fluid buildup, or inner ear damage, any of which can cause permanent hearing loss—especially if it reaches the cochlea or auditory nerve.
How long does hearing loss last after an ear infection?
Most temporary hearing loss resolves within a few days to two weeks after the infection clears. If hearing hasn’t returned after 3–4 weeks, it’s important to see an audiologist or ENT to rule out lasting damage or a persistent problem.
What are the signs of serious ear damage?
Warning signs include:
Hearing loss that doesn’t improve
Tinnitus (ringing or buzzing)
Dizziness or balance issues
Persistent ear drainage
Fullness or pressure that won’t go away
These symptoms may indicate structural or inner ear involvement and should be evaluated promptly.
Can antibiotics prevent hearing loss?
Antibiotics can treat bacterial ear infections, reducing inflammation and preventing the infection from spreading deeper into the ear. While they don’t “cure” hearing loss, timely treatment can prevent permanent damage in many cases. However, they’re ineffective against viral infections.
Are some people more at risk than others?
Yes. Higher-risk individuals include those with:
Recurrent or chronic ear infections
A history of eardrum perforation
Compromised immune systems
Chronic sinus or respiratory issues
Uncontrolled diabetes
Smokers or those exposed to secondhand smoke
Should adults get regular ear checkups?
If you’ve experienced ear infections, frequent hearing changes, or work in loud environments, yes. Routine hearing exams help catch subtle changes early and reduce the risk of permanent hearing loss due to neglect or delayed treatment.
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you are concerned about your hearing or ear health, please consult a qualified healthcare provider.






