If you’ve ever had a doctor peer into your ear with a small lighted instrument, you’ve experienced an otoscopy. This simple, quick procedure is a cornerstone of ear health—but most people don’t realize just how revealing and important it can be.
So, what is otoscopy?
In essence, it’s a visual inspection of your ear canal and eardrum, performed using a tool called an otoscope. It helps healthcare professionals detect a wide range of conditions—from wax buildup and infections to structural problems and early signs of hearing loss.
Whether you’re dealing with unexplained ear pain, frequent infections, or hearing changes, an otoscopy is often the first step to diagnosis and relief.
In this article, we’ll break down what otoscopy is, how it’s performed, what it can reveal, and why it’s so crucial for patients of all ages. You’ll learn what to expect during the exam, how modern tools have enhanced the process, and when it’s time to book one for yourself or a loved one.
Because when it comes to ear health, seeing really is believing.
What Is Otoscopy and How Does It Work?
Otoscopy is a fundamental tool in ear care, used by healthcare professionals around the world to inspect the ear canal and eardrum. Despite its simplicity, it’s an incredibly powerful method for identifying a wide range of ear-related issues.
Definition and Purpose
At its core, otoscopy is a visual examination of the outer and middle ear using a handheld device called an otoscope. This instrument has:
A light source to illuminate the ear canal
A magnifying lens to provide a clear view of the structures inside
A disposable speculum (the cone-shaped tip) that fits gently into the ear
Doctors, nurses, audiologists, and ENT specialists use otoscopy to:
Diagnose ear infections (like otitis media or swimmer’s ear)
Detect wax buildup, foreign objects, or skin conditions
Check for perforations, fluid, or inflammation
Assess healing after treatment or surgery
Monitor hearing-related symptoms like tinnitus, muffled hearing, or pressure
Types of Otoscopy
Standard Otoscopy
The most common type, used in routine checkups. The provider gently inserts the speculum and visually inspects the ear canal and eardrum.Pneumatic Otoscopy
Adds a bulb that delivers a puff of air to test eardrum movement. This helps identify fluid behind the eardrum, commonly seen in middle ear infections.Video Otoscopy
Uses a tiny camera and displays a live image on a screen—allowing patients to see inside their own ear and providing better documentation for care.
What Can Be Seen During an Otoscopy Exam?
While it may seem like a small peek into your ear, an otoscopy can reveal a surprisingly detailed picture of your ear health. Trained professionals can spot subtle signs that point to infections, structural damage, blockages, or other issues that may be impacting your comfort or hearing.
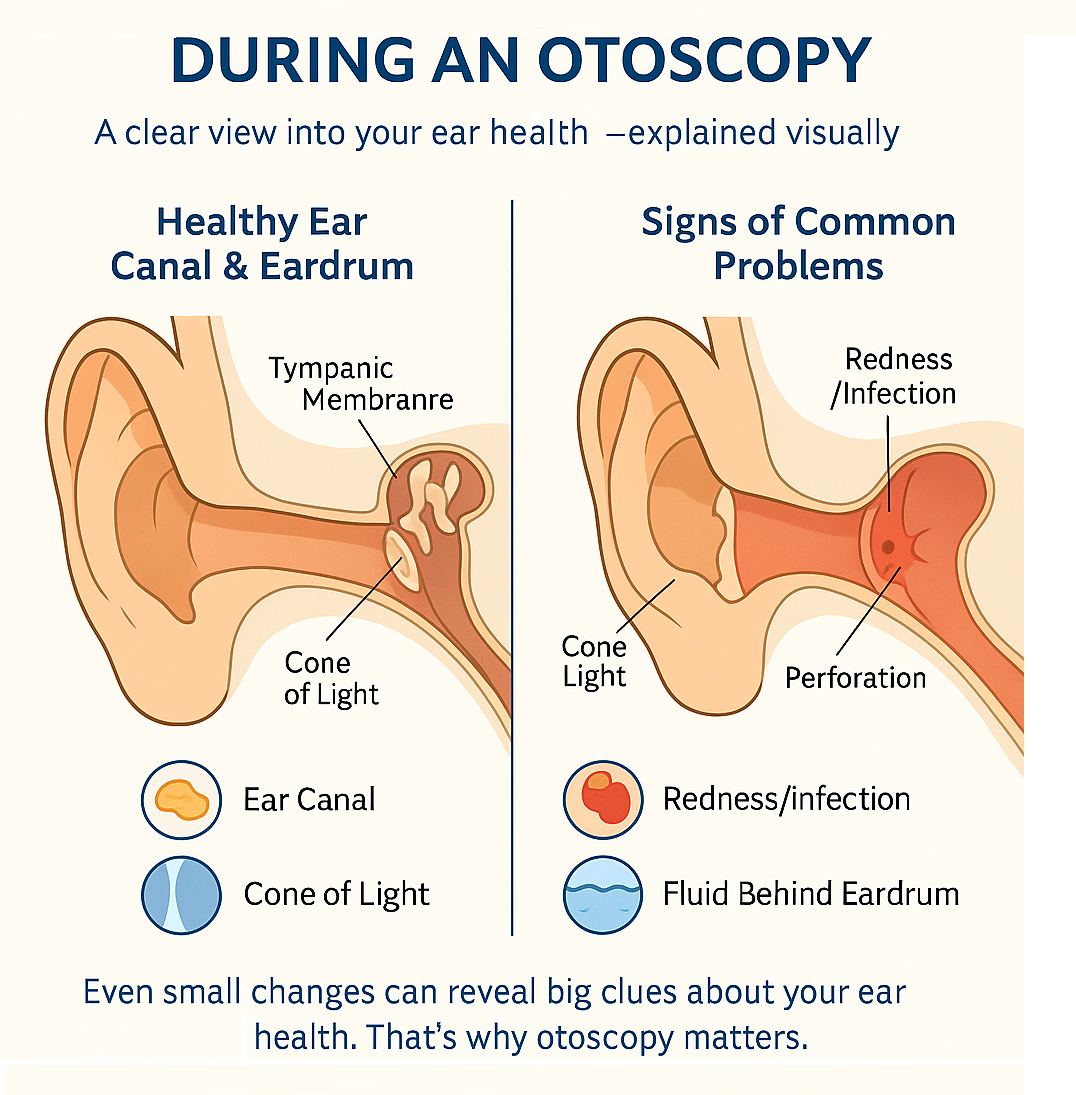
Structures Visible Through the Otoscope
During the exam, the provider will inspect:
The Ear Canal: Looking for redness, swelling, flaking skin, wax buildup, or foreign bodies
The Tympanic Membrane (Eardrum): Checking for color (healthy eardrums are pearly gray), position (bulging or retracted), and integrity (intact vs perforated)
Reflections and Landmarks: A cone of light should be visible on a healthy eardrum, along with key anatomical features like the malleus (a small bone)
Even subtle changes in these structures can reveal a lot about what’s going on in your ears—and possibly your sinuses or throat as well.
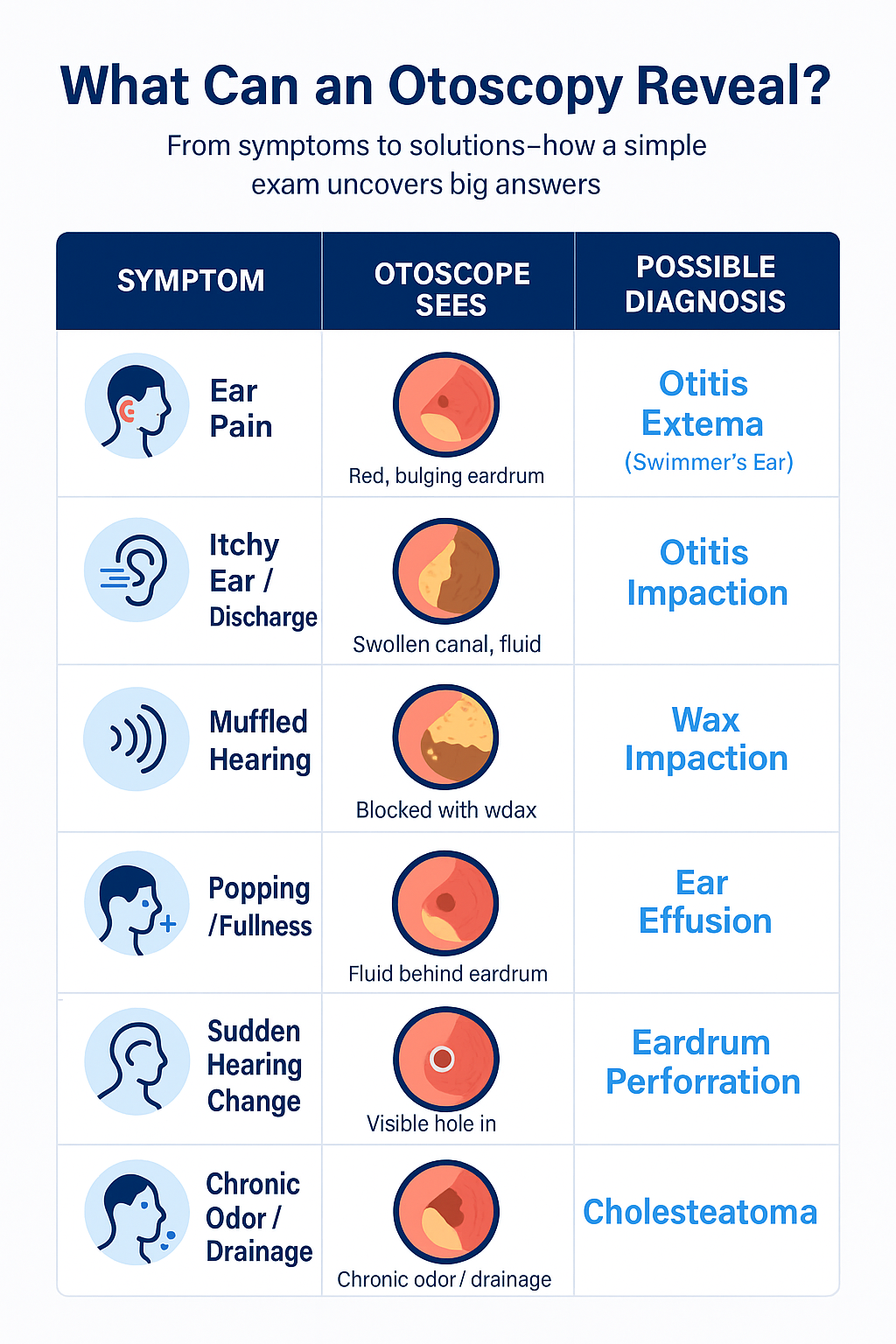
Conditions Commonly Detected
Otoscopy can detect and help diagnose:
Otitis Media (middle ear infection): Bulging or red eardrum, fluid behind the eardrum, poor movement with pneumatic otoscopy
Otitis Externa (swimmer’s ear): Red, swollen canal; discharge or tenderness
Earwax Impaction: Visible wax obstructing the canal, which may require cleaning
Eardrum Perforations: Holes or tears in the eardrum, often from trauma or infection
Cholesteatoma: Abnormal skin growth in the middle ear that may appear as a white mass
Foreign Bodies: Especially common in children, small objects may be lodged in the ear
Skin Conditions: Psoriasis, eczema, or dermatitis affecting the ear canal lining
It’s a surprisingly effective diagnostic tool—and often the first line of defense in identifying deeper hearing or infection problems.
What to Expect During an Otoscopy
Otoscopy is one of the quickest and least invasive medical exams you’ll ever experience. While it can feel a bit odd, especially the first time, it’s typically painless and over in seconds—making it ideal for patients of all ages, from toddlers to seniors.
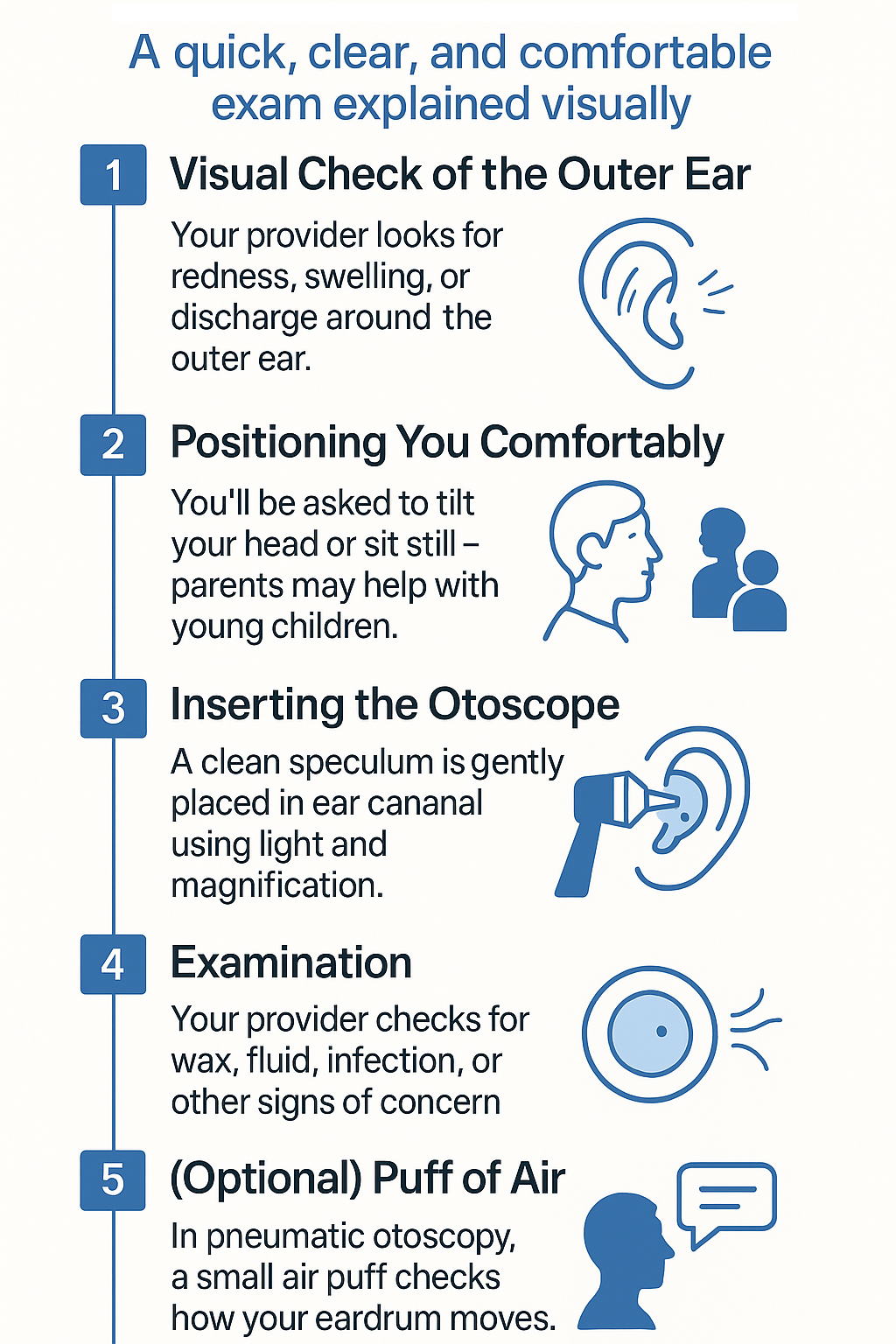
Step-by-Step Guide to the Procedure
Here’s what typically happens during an otoscopy:
Visual Inspection
Your healthcare provider will start by looking at the outside of your ear to check for redness, swelling, or signs of infection.Preparation
You’ll be asked to sit still, and the provider may gently tilt your head or ask you to turn slightly. For infants or small children, parents may be asked to help keep them secure.Insertion of the Otoscope
A fresh disposable speculum is placed on the otoscope, which is then gently inserted into your ear canal. The provider will move it slightly to get a clear view of your eardrum.Examination
Using the light and magnification, they’ll look for wax buildup, infection, fluid, or structural changes. In some cases, a puff of air is used to test eardrum movement (pneumatic otoscopy).Discussion of Findings
After the inspection, your provider will share what they saw and recommend next steps—whether that’s treatment, further testing, or simply monitoring.
Is It Painful or Uncomfortable?
For most people, otoscopy is completely painless. At most, you might feel:
A slight pressure as the speculum enters the ear
Temporary tickling or coolness from the air puff (if used)
Brief discomfort if the ear is infected, swollen, or highly sensitive
If you do feel significant pain, let the provider know—they’ll stop immediately and may adjust the approach.
Otoscopy is especially helpful in reassuring patients that their ears are healthy—or in catching problems early before they worsen.
Who Needs an Otoscopy and When?
Otoscopy isn’t just for people with earaches. It’s a crucial tool for spotting a range of ear, nose, and throat (ENT) conditions—and often plays a key role in both routine checkups and symptom-driven evaluations.
Common Symptoms That Call for Otoscopy
If you’re experiencing any of the following, an otoscopy might be your doctor’s first step:
Ear pain or pressure
Muffled hearing or sudden hearing loss
Discharge or fluid leaking from the ear
Dizziness or balance issues
Ringing in the ears (tinnitus)
Fever with cold or flu symptoms in children or adults
Itching, swelling, or visible changes in the outer ear
These signs often point to conditions like infections, wax impaction, or inflammation—all of which can be evaluated through a quick visual exam.
Routine vs Diagnostic Use
Otoscopy can be used for:
Routine Exams: Part of a general physical or pediatric checkup, especially if the patient has a history of ear issues
Diagnostic Evaluations: Triggered by specific complaints or sudden changes in hearing or comfort
Follow-Up Monitoring: To check healing after treatment for infections or after removal of foreign objects or wax
Children and Otoscopy
Kids tend to get ear infections more frequently due to the shape and development of their Eustachian tubes. Otoscopy is essential in:
Diagnosing acute otitis media
Monitoring recurrent ear infections
Checking for fluid behind the eardrum, which can affect speech development
Regular otoscopic checks can prevent small issues from becoming long-term problems, especially in growing children.
Otoscopy in Modern Practice: Tools and Technology
The classic image of a doctor peeking into an ear with a handheld scope still holds true—but technology has taken otoscopy to new heights. From enhanced visuals to patient education, digital tools are making this exam more effective and engaging than ever before.
Advances in Digital Otoscopy
Modern otoscopes are increasingly digital, offering:
High-definition imaging for clearer, more accurate assessments
Storage of images and videos in patient records for tracking changes over time
These devices are especially valuable for complex diagnoses and in telemedicine, where specialists can review images remotely.
How Video Otoscopy Is Transforming Care
Video otoscopy uses a small camera inside the speculum to project a real-time image of your ear canal and eardrum onto a screen. This serves several important purposes:
Enhances patient understanding—you can see exactly what the doctor sees
Improves documentation—great for comparing pre- and post-treatment images
Boosts diagnostic accuracy, especially for ENT specialists
It’s particularly useful for children or nervous patients, as it allows doctors to explain findings visually and reduce fear.
Portable and Consumer-Friendly Devices
There are now smartphone-compatible otoscopes and home-use models, though experts caution:
They’re useful for monitoring, not replacing medical expertise
They’re best used under the guidance of a healthcare provider
As otoscopy continues to evolve, its role as a quick, non-invasive, and highly informative exam remains unchanged—but the experience is more collaborative and precise than ever before.
Conclusion: Seeing Is Believing – How Otoscopy Supports Better Hearing and Diagnosis
For such a quick and simple exam, otoscopy offers a wealth of information. From spotting infections and wax blockages to identifying subtle changes in the eardrum, this tool gives healthcare providers a direct line of sight into your ear health—and the peace of mind that comes with it.
Whether you’re managing recurring ear issues, monitoring your child’s hearing, or simply staying proactive with your health, otoscopy plays a vital role. And with advances in video and digital technology, the experience is more patient-friendly and insightful than ever.
So the next time someone shines a light in your ear, remember—it’s not just routine. It’s a gateway to better understanding, early diagnosis, and sound solutions.
Because when it comes to your hearing, a closer look can make all the difference.
Frequently Asked Questions
Is otoscopy safe for children?
Yes—otoscopy is safe and commonly used in children. In fact, it’s a vital tool for diagnosing ear infections, fluid buildup, and wax blockages in young patients. Pediatric specialists use smaller specula and gentle techniques to minimize discomfort.
How long does an otoscopy take?
A typical otoscopy takes less than a minute per ear. The entire process—from setup to explanation of findings—usually fits into a standard GP or ENT consultation and is one of the quickest diagnostic exams available.
What if my ear hurts during the exam?
If your ear is already inflamed or infected, you might feel mild discomfort or tenderness when the speculum is inserted. Always let the provider know if something hurts—they can adjust their approach or stop the procedure if necessary.
Can I see what the doctor sees?
With video otoscopy, yes! These modern tools project a live image onto a screen so you can view your ear canal and eardrum in real time. It’s a fantastic way to better understand your condition and engage with your care plan.
Is otoscopy part of a regular hearing test?
Not always—but it’s often performed alongside hearing evaluations. Otoscopy helps rule out obstructions, infections, or structural issues that might affect hearing test results. It’s commonly used as a preliminary step before audiometric testing.
Do I need a referral for an otoscopy?
In most primary care or audiology settings, you don’t need a referral—otoscopy is part of routine care. However, if you’re being seen by an ENT specialist or seeking treatment through certain health systems, you may need a referral from your GP.
Disclaimer
This article is for informational purposes only and is not a substitute for professional medical advice, diagnosis, or treatment. If you are concerned about your hearing or ear health, please consult a qualified healthcare provider.





